Allow Me to Introduce Myself
This is my first blog on Project Lyme, so let me introduce myself. I am a physician, a board-certified internist, with a private practice in Denver, Colorado, specializing in the treatment of patients with tick-borne illness. Back in the old days—i.e., 20 years ago—those of us treating chronic Lyme disease had either suffered with Lyme disease ourselves or had a close relative who was infected. That includes me—the story of what happened to me is described in my recently released book, Recovery From Lyme: The Integrative Medicine Guide to the Diagnosis and Treatment of Tick-Borne Illness. Having suffered the ravages of Lyme, I have a very personal perspective on these illnesses.
History of Lyme
When Lyme was “discovered” in Lyme, Connecticut, the lead researcher was a rheumatologist. That made sense because they were investigating an outbreak of juvenile rheumatoid arthritis, a fairly uncommon autoimmune rheumatologic disorder. The researchers did accurately identify that these kids did not have JRA, but rather an illness transmitted by a deer tick. What they did not appreciate was the occurrence of neurological issues. In fact, Lyme Disease was identified in Europe as far back as 1909, and there were numerous reports in the European medical literature of neurological complications associated with this infection.
And that brings us to Lyme disease as a cause of mental illness. But before I delve into that important topic, I want to provide a context.
If Lyme disease is properly diagnosed and treated in its acute stage, most patients are cured. However, there are two groups of patients that become chronically ill. The first is people who were treated for acute Lyme disease but nevertheless continue to have chronic symptoms. These folks are labeled Post-Treatment Lyme Disease Syndrome (PTLDS), suggesting that their infection is eradicated and they are suffering from something else. (They aren’t—they are still infected, and I will get into that in a later post.) The second is people who never noticed a tick bite or rash—they never knew they had acute Lyme disease—but developed chronic symptoms at some point. They are typically diagnosed with Chronic Fatigue Syndrome, Fibromyalgia, an autoimmune disorder, or a mental health issue.
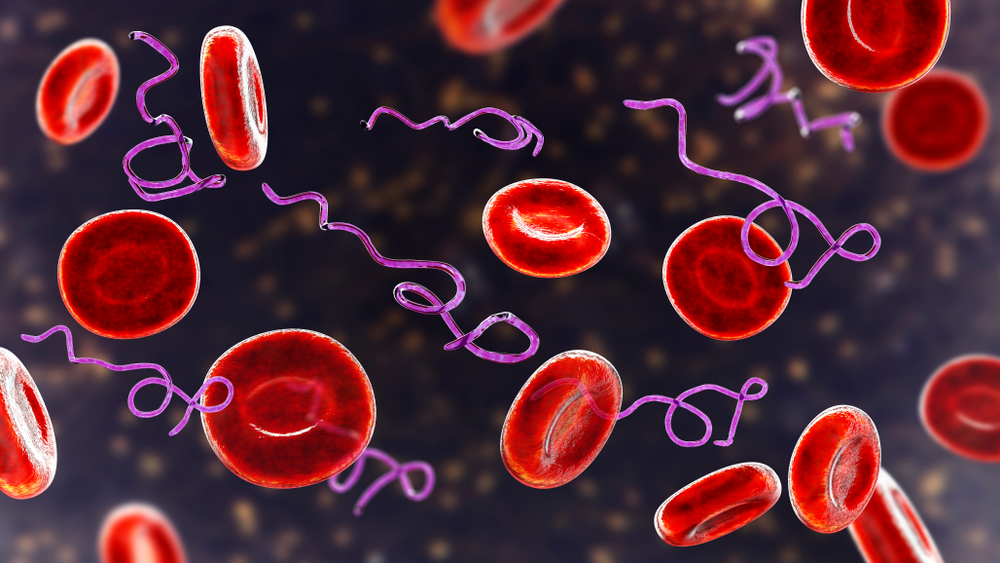
Chronic Lyme disease is not just an infection with the Lyme pathogen, Borrelia burgdorferi. The ticks are veritable cesspools of bugs, and a single tick attachment can result in the transmission of a handful of different microbes. All my patients with chronic Lyme have these coinfections, and they make the symptoms worse and the illness more difficult to treat. In addition, chronic infection and chronic inflammation lead to hormone imbalances, sensitization syndromes (like food sensitivities, mold allergy and multiple chemical sensitivities), autoimmunity and detoxification problems. I prefer to use the term Lyme disease complex, since it acknowledges that there is a lot more going on than infection with the Lyme bug.
Patient Case Study
Here’s an example. A pleasant 39-year-old female nurse, Ann was experiencing severe anxiety and depression. These symptoms came on fairly suddenly. But she also had the simultaneous onset of a handful of somatic complaints: facial pain, headaches, palpitations, joint pains, low grade fevers, night sweats, pins and needles sensation and fatigue. Ann tried three different antidepressants that were prescribed for her but she couldn’t tolerate them. Her husband was convinced that she was “nuts.”
I saw Ann a few years into her illness. She turned out to be infected both with the Lyme bacteria and with Babesia, a common coinfection. Further evaluation revealed that she also had low adrenal and pituitary hormones, had developed some food sensitivities, and had detoxification issues. But after two years of treatment, she was in full remission and off all medications. During the past six years, Ann has not only remained asymptomatic, but she also has made herself available to talk with folks who are still struggling. Her husband became a believer.
Her husband was convinced she was nuts.
Lyme’s Psychiatric Symptoms
The point here is that these bugs can cause psychiatric symptoms—really bad ones. These symptoms can predominate and overwhelm the physical complaints. It turns out that Amy was not anxious and depressed because she was otherwise ill, or stressed out by her work or her marriage. The infections were causing her psychiatric symptoms. Microbes can cause mental illness.
Here is a list of neuropsychiatric issues associated with Lyme disease:
- Anxiety, agitation, panic attacks, phobias
- Depression
- Irritability, anger, oppositional, rage
- Obsessive-compulsive disorder
- Bipolar disorder
- Eating disorders
- Anhedonia—inability to feel joy
- Dissociative episodes—a sense of not being present or in their bodies
- Psychosis
- Personality syndromes
- Addiction disorders
These psychiatric symptoms are often the most severe complaints in these patients, like Ann. The most common cause of death in folks with Lyme disease complex is suicide. But only rarely are the mental health issues the only complaints. There is a long list of potential symptoms, but most patients complain of impaired cognition (“brain fog”), fatigue, headaches, neck pain, sleep issues and joint and/or muscle pain.
Additional Resources
This is just an introduction. Mental health issues caused by microbial infections turn out to be quite common, and mostly undiagnosed. In subsequent blogs I will be covering important topics like PANS/PANDAS and eating disorders.
If you are interested in doing some reading on your own, I suggest:
Bransfield R. Neuropsychiatric Lyme Borreliosis: An Overview with a Focus on a Specialty Psychiatrist’s Clinical Practice. Healthcare (Basel). 2018;6(104):1–23.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6165408/
My book: Recovery From Lyme: The Integrative Medicine Guide to the Diagnosis and Treatment of Lyme Disease (Skyhorse Press, 2021)