Treatment
Treating Lyme With Antibiotics
There is no universally effective treatment for Lyme disease. Prescribed medication will vary from person to person and should be monitored by a medical provider. This resource is designed to educate patients and caretakers about the antibiotics commonly used to treat Lyme. It leverages existing treatment guidelines and expert opinions to provide information about stages of care, types of antibiotics, typical dosages, side effects, and emerging research. This resource should not be misconstrued as medical advice. For Project Lyme’s full disclaimer, see here.


Introducing Antibiotic Treatment
Doctors will likely prescribe antibiotics as a first step to treating your infection. Which antibiotic, and for how long, will depend on a variety of factors including the duration of the infection, the severity of illness, the presence of co-infections, individual immune health deficiencies, age, weight, and patient tolerance.
Stages of Care
Antibiotics are typically administered orally, but in appropriate cases, they may also be taken intravenously or intramuscularly. Oral antibiotics are standard protocol for early stages and uncomplicated cases. Intravenous (IV) antibiotics may be used if the disease is impacting the central nervous system or cardiac function, if the patient does not tolerate oral antibiotics, or if a particular medication is only offered intravenously. Intramuscular (IM) antibiotics may be used if a person can not easily swallow pills, has gastrointestinal dysfunction, or is pregnant. For example, IM benzathine penicillin is a long-acting antibiotic and has 24-hour coverage during pregnancy for those wanting extra protection against possible maternal-fetal transmission of Lyme disease.
Treatment is typically prescribed considering your known exposure, potential co-infections, response to treatment, and severity of illness. There are four stages of care, which range from preventative treatment to chronic cases.
PROPHYLAXIS — If you find an attached tick, it is very important to properly remove it, store it in a zip lock bag with a moist paper towel or cotton ball for testing, and see a doctor as soon as possible to obtain a preventative course of antibiotics. Prescribed treatment will be based on a variety of factors, including the type of tick, whether it came from an endemic area, how it was removed, and the estimated length of attachment. The risk of transmission is greater if the tick is engorged, or if it was not removed properly. Early preventative treatment will help your body stave off the infection before it becomes disseminated and harder to eradicate. Ideally, this prophylactic treatment will help the patient avoid reaching the symptomatic stage.
- Treatment recommendations: Adults and children at this stage are typically prescribed 4-6 weeks of oral antibiotic therapy. For adults, Lyme specialists recommend 200 mg of doxycycline taken twice per day. Please be aware that many general practitioners will prescribe 100mg, but our view is that 200mg is more advisable. Children over age 8 are also commonly prescribed doxycycline based on weight, up to 200 mg taken twice per day. A newer study suggests that doxycycline does not present a significant risk of staining unerupted teeth in younger children (typically under the age of 8). Amoxicillin may be prescribed to pregnant women (1g every 6 hours) or children under age 8 (50 mg/kg/day every eight hours). Cephalosporins like cefuroxime axetil and cefdinir are also possible choices during pregnancy or for young children, taken twice a day, based on weight. With any tick bite it is always important to remember the possibility of co-infections, so make sure to test the tick for other Borrelia strains (i.e., Borrelia miyamotoi), as well as Babesia spp (i.e., B. microti and B. duncani), Bartonella spp (note that tick transmission is debated), Anaplasma, Ehrlichia, other rickettsial infections (i.e., Rocky Mountain Spotted Fever, Q-fever), tularemia and tick-borne viruses (i.e., Powassan virus, Heartland virus, Bourbon virus).
EARLY LOCALIZED LYME — Patients at this stage present with a single erythema migrans rash but no other constitutional symptoms.
- Treatment recommendations: Adults are typically prescribed oral therapy that is continued until symptoms subside for at least one month, with a 6-week minimum dosage. For adults, Lyme specialists recommend 200 mg of doxycycline taken twice per day. If Rocky Mountain Spotted Fever is suspected, then doxycycline is prescribed regardless of age. In lieu of doxycycline, children under age 8 may be prescribed amoxicillin based on body weight (50 mg/kg/day every eight hours). Cephalosporins like cefuroxime axetil and cefdinir are also possible choices for young children, taken twice a day, based on weight (125 to 500 mg every 12 hours). Pregnant women in the 1st and 2nd trimesters may be given IV antibiotics for 30 days, then oral for 6 weeks in the 3rd trimester. Intramuscular antibiotics in pregnancy (penicillins, cephalosporins) may also be considered.
EARLY DISSEMINATED LYME — At this stage, patients may present with symptoms of early-stage Lyme, such as flu-like symptoms, joint pain, or facial drooping known as Bell’s palsy.
- Treatment recommendations: If a patient is symptomatic for less than one year, doctors will typically prescribe adults 200 mg of doxycycline, taken twice per day for 4 to 8 weeks, or until symptoms are no longer present for at least a month. Lyme specialists may also add an antibiotic that is more effective against the Lyme persister cells, such as tinidazole, dosed by weight. Often, treatment will last 4-6 months but may take longer depending on individual response to treatment. Newer peer-reviewed protocols indicate that 8 weeks of a persister drug regimen like dapsone combination therapy utilizing biofilm agents may lead to long-term remission in approximately 50% of individuals if there are no active co-infections, like Babesia and/or Bartonella. Pregnant women are usually treated the same as in early localized Lyme, but treatment will continue throughout pregnancy. Children are also normally prescribed oral therapy similar to early localized Lyme with duration based upon clinical response. Patients who are more ill or not tolerating their oral protocols may be prescribed IV therapy (or occasionally IM therapy) in place of an oral regimen. Longer courses of IV therapy may be necessary if symptoms persist, if there is involvement of the central nervous system (i.e., stiff neck, headache, light and/or sound sensitivity, dizziness, cognitive difficulties, new onset neuropsychiatric symptoms), if there is peripheral nervous system involvement (i.e., tingling, numbness, burning, and/or stabbing sensations of the hands, limbs, feet known as neuropathy), or if there are cardiological symptoms (irregular heart rhythm or inflammation of the heart).
LATE DISSEMINATED LYME — If symptoms have been present for greater than one year, or if you have received prior therapy for Lyme disease, then other potentially contributing causes such as co-infections, mold, autonomic dysfunction, mitochondrial dysfunction, mast cell activation, and autoimmunity should be explored as part of the differential diagnosis. Patients with persistent Lyme symptoms will often need longer treatment courses and combination therapies to address co-infections, biofilms, and stationary phase Borrelia.
- Treatment recommendations: Adults and children can expect to be in treatment for 14 or more weeks, preferably under the guidance of a Lyme disease specialist. Protocols will typically involve individualized combination therapy with at least two dissimilar antibiotics to address both fast replicating and persister forms of Borrelia, as well as biofilms. Emerging published regimens using dapsone combination therapy for 8 weeks have shown efficacy in late disseminated Lyme, putting roughly 50% of long-term Lyme patients into remission. This option should be discussed with your prescribing physician before undergoing longer-term oral, IM, or IV therapy.
Antibiotic Classes
There are various classes of antibiotics generally accepted for use in the treatment of Lyme disease. Since all antibiotics can promote yeast overgrowth, taking nystatin and a low carbohydrate diet with sufficient probiotics may be recommended to avoid antibiotic-associated diarrhea.
- TETRACYCLINES include the most commonly prescribed antibiotic, doxycycline, as well as minocycline. Dosages that have been published to be effective include up to 200 mg of minocycline twice a day, and/or doxycycline 200 mg twice a day. Minocycline is more highly lipid soluble than doxycycline and has excellent CSF penetration, making it potentially useful in treating Lyme neuroborreliosis. However, at higher doses, minocycline may cause vestibular symptoms (dizziness, off balance, vertigo) in some patients. Lower doses may still be effective when used in combination with rifampin/rifabutin and dapsone, along with hydroxychloroquine (Plaquenil) and multiple biofilm agents. Tetracyclines are also typically prescribed to treat tickborne rickettsial infections such as Ehrlichia, Anaplasma, and Rocky Spotted Mountain Fever.
- PENICILLINS such as amoxicillin are another option that your medical provider may prescribe. Unlike tetracyclines, penicillins require sustained bactericidal levels for at least 72 hours to be effective. If you prefer intramuscular injections, benzathine penicillin (“Bicillin-LA”) may be a good option. The doses are relatively small and the sustained blood and tissue bactericidal levels make this an effective alternative.
- CEPHALOSPORINS are another commonly prescribed antibiotic, but will only be effective in their 2nd or 3rd generations. These antibiotics have been shown to be effective in penicillin and tetracycline failures or in combination with other antibiotics. IV ceftriaxone (Rocephin) may be prescribed to treat Lyme carditis or neurological Lyme. Typically cephalosporins are administered twice daily orally or once daily intravenously.
- MACROLIDES include drugs like erythromycin, azalide, azithromycin, and clarithromycin. Given their ineffectiveness as a monotherapy, they have been utilized in combination therapies and are typically administered concurrently with hydroxychloroquine or amantadine, which raises vacuolar pH. This may affect your QT interval on an electrocardiogram, potentially causing arrhythmias. An EKG should be obtained before taking macrolides, especially if used in combination with other medications that can affect the QT interval (i.e., PPIs, SSRIs, many psychiatric medications, nausea medication like Zofran, or hydroxychloroquine). These drugs may also be given by intravenous, intramuscular, or subcutaneous injection, which has shown excellent results but typically causes abrupt Jarisch-Herxheimer reactions in patients.
- ANTIMYCOBACTERIALS include drugs such as rifampin and rifabutin. Rifampin has been studied in combination with other antibiotics. It has been utilized to reduce the protective layer of Borrelia and was able to penetrate biofilms, which may otherwise allow the infection to persist. Prescriptions of rifampin are typically around 300 mg orally twice a day in adults, with lower doses in children based on body weight (150 mg orally twice daily). Antimycobacterials are often used to treat Bartonellosis, in combination with other antibiotics. *It is important to note drugs in this class may interfere with the regulation of many other drugs. For example, studies and case reports have demonstrated that rifampin accelerates the metabolism of several drugs, including oral anticoagulants, oral contraceptives, glucocorticoids, digitoxin, quinidine, methadone, hypoglycemics, and barbiturates.
- SULFONES are a class of antibiotics that include the drug dapsone. Currently, there are a total of seven published dapsone studies in approximately 365 patients, making it a hot-button topic in the Lyme community. Dr. Richard Horowitz published this “Double Dapsone Protocol,” which showed promising results in an 8-week of double dose dapsone protocol. The study showed that roughly 50% of patients achieved long-term remission if active Babesia and Bartonella were not present. Dosages start at 25 mg every other day or every day, gradually increasing to 100 mg twice per day, based upon patient response and tolerance. Dapsone has been used in combination with hydroxychloroquine, a tetracycline, and/or rifampin (occasionally with Zithromax and methylene blue to help increase efficacy against Bartonella “persisters”). To learn more details on the efficacy of this protocol, see Dr. Horowitz’s article and this Project Lyme interview here. For resistant Bartonella infections, high-dose dapsone combination therapy may represent a novel treatment regimen, but more clinical studies and dosage regimens are required to determine long-term clinical efficacy.
Side Effects
All of the antibiotics listed above can cause side effects. Some are avoidable but some may require additional treatment if they occur. Side effects of antibiotics include:
- A lower white blood cell count, which will return to normal over time
- Mild to severe diarrhea, which can be resolved or prevented by using a high-quality probiotic, taken hours before or after antibiotics
- Sensitive skin and rashes. If these occur, speak with your doctor.
- A Herxheimer reaction, meaning symptoms may worsen and then dissipate
- Infection with other antibiotic-resistant organisms unrelated to Lyme
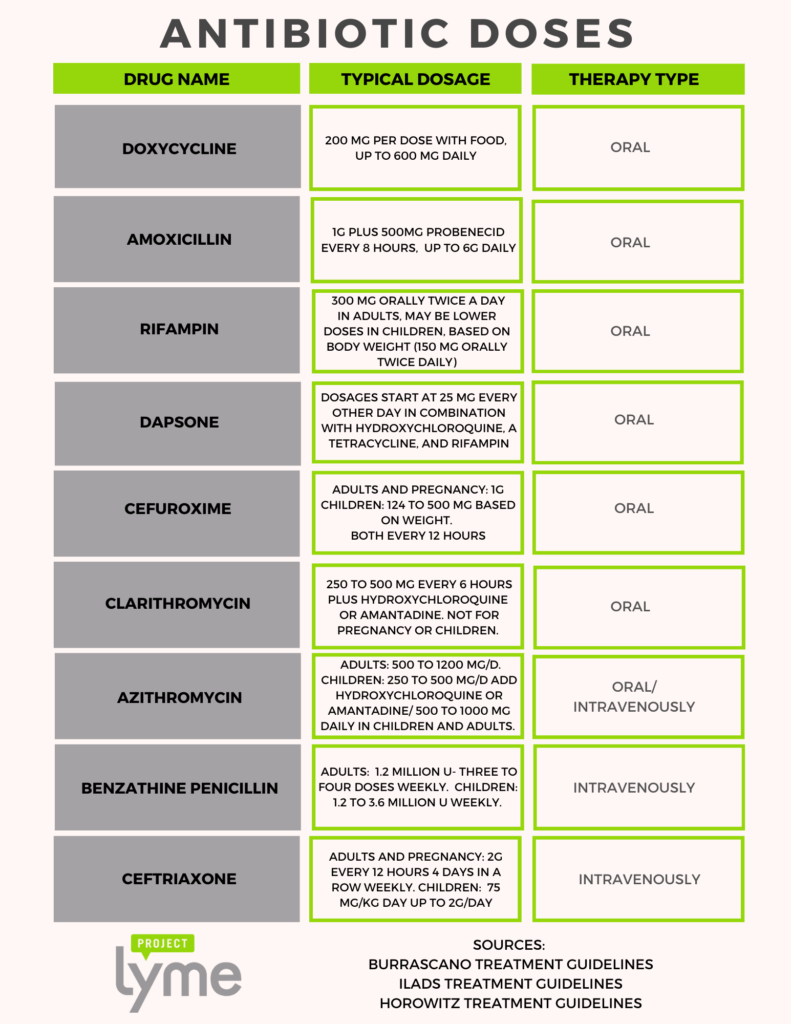
Typical Antibiotic Dosages
This is not meant to be an exhaustive list. Combinations and antibiotic names or dosages may vary.
Emerging Treatments
As previously stated, there is no universally effective treatment for persistent Lyme disease. Unfortunately, despite the prevalence of Lyme disease, there has been very little funding to support the development of more effective protocols. Lyme non-profit organizations, including Project Lyme, have funded groundbreaking research to identify novel treatments. Note that the therapies listed below have been the subject of preliminary research, but need additional study before they will become generally accepted in use for Lyme disease by the medical community.
- Daptomycin is an antibiotic that has been utilized recently in combination therapies. For example, in this study through Johns Hopkins, when combined with doxycycline and ceftriaxone, daptomycin effectively cleared Lyme disease infection in vitro as well as in mice. However, daptomycin is relatively expensive and only available intravenously.
- Disulfiram is a medication that has typically been used to help those suffering from alcohol addiction. Stanford University researchers published a study that it can act as a “persister” drug similar to dapsone to eradicate stationary phase borrelia. Dr. Kenneth Leigner has also published studies on its potential use. Potential side effects include significant fatigue, neuropathy, liver function abnormalities, and psychiatric effects at the full dose (500 mg). The 6-18 month regimen has approximately a 36% long-term remission rate.
- Hygromycin A is a long-existing antibiotic that has recently been found to selectively kill Borrelia bacteria. The antibiotic was able to treat Lyme disease in mice trials without disrupting the microbiome, which is one of the main side effects of existing treatments. Project Lyme has granted money to license this antibiotic and help bring it to market.
- Nitroxoline was recently studied and showed that this antibiotic long used to treat urinary tract infections was proven to be very effective at combating biofilm infections in Europe. It was also found to be more active than doxycycline and equally active as cefuroxime (standard Lyme disease antibiotics) against the Lyme bacteria, B. burgdorferi. More importantly, nitroxoline two-drug combinations, nitroxoline + cefuroxime and nitroxoline + clarithromycin, as well as the nitroxoline three-drug combination, nitroxoline + cefuroxime + clarithromycin, were as effective as the persister drug daptomycin-based, positive control three-drug combination, cefuroxime + doxycycline + daptomycin, completely eradicating stationary-phase B. burgdorferi in the drug-exposure experiments and preventing regrowth in the subculture study. While this research is promising, further studies are needed to test nitroxoline’s effectiveness in animal and human subjects. This antibiotic is not currently available in the United States.
Additional Resources
For more information on antibiotics and treatment guidelines, see the resources listed below.
- Burrascano’s Treatment Guidelines
- ILADS Treatment Guidelines
- Johns Hopkins Lyme Disease Research Center
- Columbia Lyme and Tick-Borne Diseases Research Center
Horowitz Dapsone Studies
- Efficacy of Short-Term High Dose Pulsed Dapsone Combination Therapy in the Treatment of Chronic Lyme Disease/Post-Treatment Lyme Disease Syndrome (PTLDS) and Associated Co-Infections: A Report of Three Cases and Literature Review
- Efficacy of Double-Dose Dapsone Combination Therapy in the Treatment of Chronic Lyme Disease/Post-Treatment Lyme Disease Syndrome (PTLDS) and Associated Co-infections: A Report of Three Cases and Retrospective Chart Review
- Effect of dapsone alone and in combination with intracellular antibiotics against the biofilm form of B. burgdorferi | BMC Research Notes
- Precision medicine: retrospective chart review and data analysis of 200 patients on dapsone combination therapy for chronic Lyme disease/post-treatment Lyme disease syndrome: part 1
- Precision Medicine: The Role of the MSIDS Model in Defining, Diagnosing, and Treating Chronic Lyme Disease/Post Treatment Lyme Disease Syndrome and Other Chronic Illness: Part 2

