Diagnosis
Diagnosing Lyme Disease in Children
Children are at the greatest risk of contracting Lyme disease. This resource is designed to help parents identify infections and learn more about treatment protocols, with the goal of avoiding long-term illness.


How Can Children Contract Lyme Disease?
Tick Bites
Not all ticks carry infections, but an increasing percentage do. In addition to Lyme disease, ticks can also transmit other viral, bacterial, and parasitic infections. As such, it is important to take steps to prevent a tick from attaching in the first place. Ensure your child avoids tick-infested areas, walks in the middle of trails, treats skin, clothing, and gear with appropriate repellants, and tucks pants into socks. Anytime your child comes in from the outdoors, search for and properly remove any ticks, store them in a zip lock bag with a moist paper towel or cotton ball, and send the ticks for testing. Considering it can take weeks for tests to detect measurable antibodies and the risks of disseminated infection, the medical care provider and parent should carefully weigh the risks and benefits of prophylactic antibiotic treatment in the case of a known tick bite, even before symptoms appear.
Congenital Lyme
Lyme Borrelia and other tickborne infections may be transmitted from mother to child during pregnancy. . How often this happens and the impacts on the child’s health are not well-established; however, studies show significantly fewer adverse outcomes when the mother is treated with antibiotics during pregnancy as prescribed by a Lyme specialist.
We also recommend for women of childbearing age who have been diagnosed with clusters of symptoms such as fibromyalgia, myalgic encephalomyelitis/chronic fatigue syndrome, autoimmune conditions, unexplained inflammation, unexplained immune deficiencies, psychiatric conditions such as depression or anxiety, joint pain or muscle pain to carefully consider Lyme disease as part of the differential diagnosis, preferably under the guidance of a knowledgeable provider using more reliable tests.
Identifying Infection
Symptoms
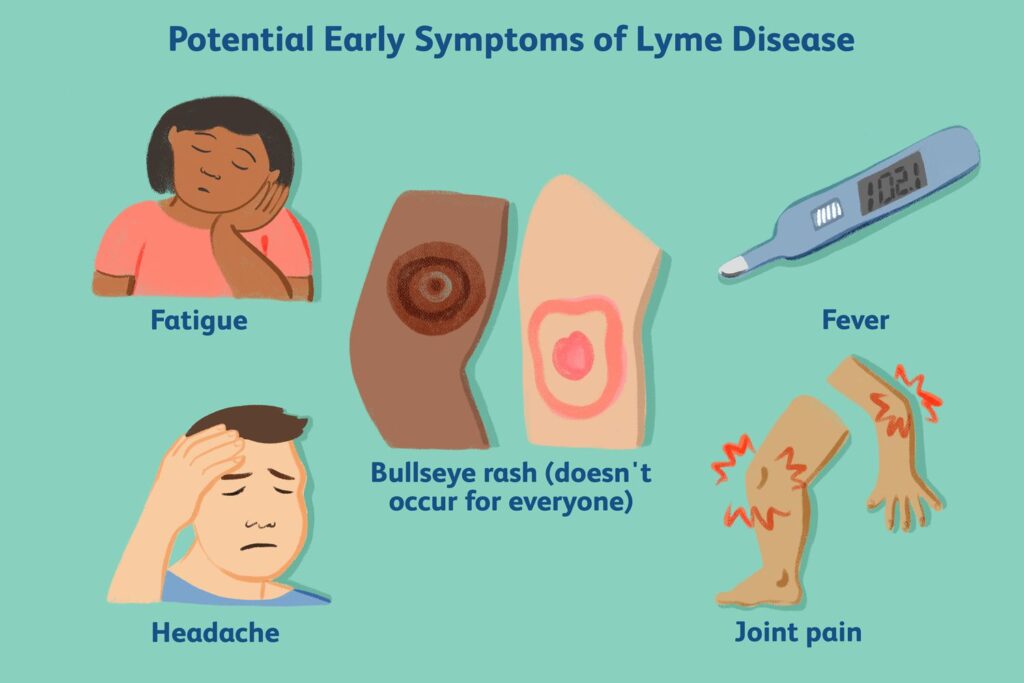
Early signs of Lyme disease include flu-like symptoms, such as fever, chills, head and neck pain, body aches (muscle and joint), malaise, and fatigue. Given that children may have a harder time conveying how and what they are feeling, these symptoms may be mistaken for irritability or viral infections, such as the flu or COVID.
A rash can also be a clear sign of Lyme disease. However, only 27% to 80% of patients will present with a rash, with a lesser percentage developing the classic “bulls-eye” rash. It is especially important to check the scalp and skin-fold areas (groin, armpits, behind the knees, and ears) so that a rash isn’t missed.
Other symptoms of Lyme disease include:
- Weakness or paralysis of facial muscles (Bell’s palsy)
- Fatigue
- Joint pain or swelling
- Muscle pain and weakness
- Migraine and non-migraine headaches
- Numbness, tingling, or weakness in extremities (neuropathy)
- Cardiac rhythm abnormalities)
- Fevers and night sweats
- Sleep disturbances
- Gastrointestinal issues (nausea, abdominal pain, vomiting, loss of appetite, gastroparesis (stomach paralysis), and/or constipation)
- Urinary problems
- Irritability and impulsivity
- Mood swings, emotional liability
- Obsessive-compulsive behaviors
- Bursts of aggression/rage
- Brain fog
- Light, sound, touch, and taste sensitivity
- Eye issues (posterior cataracts, myopia, astigmatism, conjunctival erythema, optic nerve atrophy, and optic neuritis and/or uveitis)
Children born with Lyme disease may also present with symptoms such as irritability (colic), gastroesophageal reflux with vomiting and coughing, frequent upper respiratory tract infections and ear infections, and/or developmental delays, including language, speech problems, and hypotonia.
Testing and Diagnosis
It can be difficult to determine who has a tick-borne illness. Laboratories have varying levels of sensitivity, specificity, and cost, which you can learn more about in this resource. Ultimately, a diagnosis needs to be made based on a multifaceted clinical evaluation. Most practitioners will look at medical history, conduct a physical exam, and use diagnostic testing for other potential explanations besides Lyme disease to come to a conclusion on clinical diagnosis.
Treating Infection
The way a provider will treat infection in children is dependent on several factors, including age, weight, and dissemination of infection.
Children over age 8 are also commonly prescribed doxycycline based on weight, up to 200 mg taken twice per day. A newer study suggests that doxycycline does not present a significant risk of staining unerupted teeth in younger children (typically under the age of 8). Hence, the American Academy of Pediatrics now says doxycycline can safely be used in children under 8 years for short durations, up to 21 days.
In lieu of doxycycline, children under age 8 may be prescribed amoxicillin based on body weight (50 mg/kg/day every eight hours). Cephalosporins like cefuroxime axetil and cefdinir are also possible choices for young children and can be taken twice a day, based on weight (125 to 500 mg every 12 hours). If Rocky Mountain Spotted Fever is suspected, then doxycycline is prescribed regardless of age.
For further dissemination that has caused acute central nervous system issues such as Lyme meningitis, physicians may recommend intravenous antibiotics (typically ceftriaxone), which more effectively reach therapeutic drug levels in the brain and central nervous system.
See also Treating Lyme With Antibiotics.

