Gaslighting is a manipulation technique designed to make someone doubt their own perception of reality. The psychological concept of gaslighting was first introduced in the 1944 noir-thriller Gaslight (adapted from Patrick Hamilton’s 1938 play), about newlywed Paula whose husband is trying to drive her out of her mind so he can steal a fortune in jewels hidden somewhere in the house she inherited from her dead aunt. The term “gaslighting” has become so popular in recent years that it was pronounced Merriam-Webster’s word of the year for 2022.
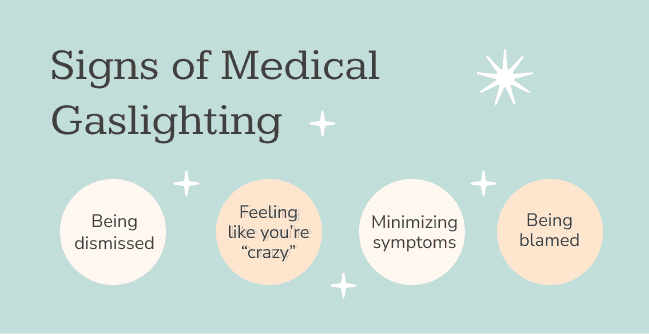
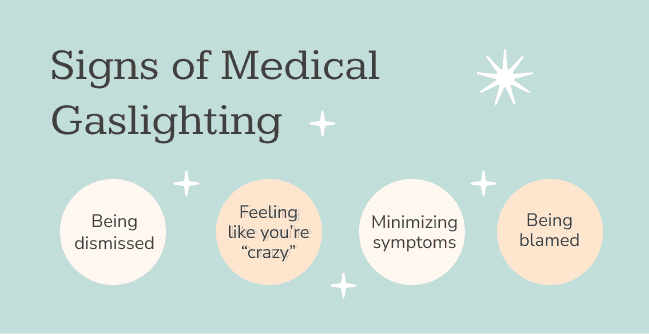
While many people are used to thinking about gaslighting in terms of personal relationships, they may not realize that it can also creep into the physician-patient dynamic and become medical gaslighting. The physician might dismiss the patient’s symptoms outright as a cry for attention or try to convince them that the pain they are experiencing is all in their head (aka psychosomatic). Many physicians are trained in medical school to look for common diagnoses that fit patients’ symptoms, so they are likely to miss or fail to consider all the other possibilities, such as Lyme disease or other vector-borne infections. This can have harmful long-term consequences, including misdiagnosis and delayed treatment.
Project Lyme recently chatted with Ashley Baker to get a patient’s perspective on medical gaslighting. Ashley is a passionate artist, Lyme disease advocate, member of Project Lyme’s Junior Board, and also one of the stories featured in the new Lyme documentary I’m Not Crazy, I’m Sick. She recalls some of her worst experiences:
In the beginning, it was like that’s all it was: medical gaslighting. Especially because for me, I didn’t get bitten by a tick and then fell ill or anything like that. I just randomly hurt myself at work. I tore my knee. When that happened, my immune system was trying to fix my knee, and it caused a flare of an infection that I didn’t even know was dormant. So for everybody, of course, they’re looking at me crazy, like: “Lyme disease? Did you even get bit by a tick? Did you have a bull’s-eye rash?” Of course, the answer is no and no, because I don’t remember either of those things. So they look at you like, well then it’s probably not Lyme disease. It’s probably a laundry list of things which I’ve been misdiagnosed with.
Chronic fatigue syndrome was one of the first, and then from there it went to fibromyalgia. And it was almost like since they didn’t have a diagnosis, they were eager to find something that filled those symptoms, even if it didn’t quite make sense or have an explanation. After I’d had 9 or 10 months of testing, going back and forth between specialists, I had one of the worst experiences I ever had with medical gaslighting.
After my primary doctor exhausted all of her resources and referrals, she sent me to a bacterial infection specialist. And at first I was excited about that, because I’m thinking OK, he’s a specialist. He understands bacterial infection. But when it comes to Lyme disease, most doctors only get a paragraph of training in med school, and it’s the typical doxycycline early stage—nobody talks about late stage. And I remember sitting in the room, just feeling defeated, and he basically was like, “You know, you have Lyme disease, but they didn’t catch the infection early. So basically you have something called “Post-Treatment Lyme Disease Syndrome.” And I didn’t understand.
I asked, “So there’s Lyme in my blood?”
“Yeah.”
“So you’re not going to treat me for the Lyme in my blood? You’re just saying I have post symptoms. What’s the treatment for that?”
“Typically, it’s cognitive therapy, yoga, meditation.”
He was telling me literally go see a therapist about the infection that he just said spread through my body that there’s not really a treatment for. And I threw a fit about it, honestly. I caused a big scene, and I was alone. I went to a lot of doctor’s appointments by myself just because of family issues that were going on when I was really sick. Being by yourself in that situation can feel really vulnerable. And I just didn’t accept it. I’m like, I can’t accept this advice from you right now.
He took me out of the patient room to his office and pulled up the chapter he had on Lyme disease from 2006. And he was just showing me, “Look, I’m not just making this up. This is what the treatment plan says.”
That experience really hurt. I left there feeling very non-validated, and I had no treatment plan. Maybe a month after that is when I started doing my own research and tapping into groups online. And from there I was able to find my current doctor that I’m with now, and that really changed my life. He just validated all those feelings that I had that whole time that were being dismissed, and I was being told it was something else, or I had to do something else to fix it.
With the medical gaslighting comes general gaslighting: people that just don’t get it. I’ve had some really bad situations where, after I’ve expressed how hard things are with Lyme, even really respected people in my community have said, “You don’t have Lyme disease.” And it’s horrible to look somebody in the face who lost their job and most of their livelihood in their twenties to a disease and say, “You don’t have it.” It’s pretty dehumanizing.
So what can someone do to minimize the fallout from medical gaslighting? Ashley encourages fellow Lyme patients to have confidence in themselves and prioritize their mental health:
You know yourself better than anybody else. Doctors are educated on a variety of topics. But at the end of the day, you are the one that is going to become the expert on that ailment or disease that you’re dealing with every day. So don’t let what somebody else says be your end-all. Don’t let what they say hold so much weight in your life that you dismiss your own voice in your head or in your heart telling you that something else is going on.
Mental stamina is so important. Taking that time to check in with yourself because other people can sometimes make you feel crazy or question yourself. So it’s trying to keep that mental health part together, because it’s not just inflammation: You’re mentally dealing with depression and anxiety, and then you have these people dismissing your experience. That’s enough to really push somebody over the edge. That’s why I could definitely resonate with people that get to that point where they feel really in a dark place, but it’s important to remember through your experience that you’re the only one who can really express the pain and the things that you’re going through.
Ashley adds that taking time for self-care can help people recover from experiences with medical gaslighting, whether from physicians or from friends and family:
Not only do I write music—which is very therapeutic for me, that’s always been my go-to thing—but I perform the music. I record it; I do music videos for it. I do a lot of different stuff that just helps me detach from the negativity in my life. I feel more grounded when I have those ways to express myself.
And that’s another thing, too: just taking some time for self-care. Sometimes I feel this pressure as a Lyme patient to overachieve all the time. I almost feel like I’m on borrowed time or that I have to make up for the time that I missed. And I’ve been trying to get myself out of that mindset because it’s actually damaging.
Medical gaslighting is unfortunately common and can be quite costly for patients, both financially and emotionally. Our hope is that as more people step forward to share their stories, healthcare professionals will shift their mindset, listen better, and be more open to different diagnoses instead of automatically dismissing patients’ concerns.