Assistance
Managing Your Mental Health
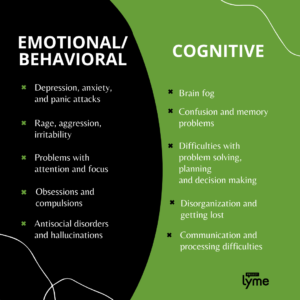
Lyme disease can impact the brain and nervous system. Some patients may experience neuropsychiatric involvement from factors, such as brain inflammation, poor sleep, and the presence of coinfections. Several psychiatric symptoms have been linked to Lyme, including depression, anxiety, panic attacks, bipolar disorder, obsessive-compulsive disorder, and more.


What are the Causes of Psychiatric Symptoms?
Lyme disease, known as the great imitator, showcases a variety of physical symptoms in patients. Much less known, however, is that it has also been proven to cause a myriad of psychiatric symptoms. According to ILADS, “Patients with late-stage Lyme and tick-borne infections may present with a variety of neurological and psychiatric problems, ranging from mild to severe.” It is also important to remember that emotional and/or cognitive disorders can sometimes be the only symptoms of Lyme disease.
One major psychiatric symptom is depression, which has been reported in 8-45% of patients with post-treatment Lyme. The graphic below outlines the full range of issues attributed to psychiatric Lyme disease, and the rest of the resource will guide you on how to identify and manage these symptoms.
How Can You Identify Your Symptoms?
Monitor Your Behavior
Just like the physical symptoms of Lyme, psychiatric symptoms can be monitored by keeping a daily journal. This practice will be helpful for you and your healthcare provider to better identify the underlying cause of your symptoms. Reflecting on things that occur throughout your day will indicate which type of psychiatric issues you may be experiencing and provide a better basis to develop effective treatment protocols moving forward.
For example, noting constant changes in your appetite, energy levels, or mood is a key indicator of depression or anxiety. Noting whether you had an outburst of rage, felt like you struggled in social settings, or were easily irritated is an example of behavioral issues caused by the psychiatric symptoms of Lyme. If you continually feel confused, feel like you can’t communicate, or experience brain fog, then this may be a result of cognitive impairment from Lyme disease.
Try a Self-Screening Tool
Self-screening can be another helpful way to understand your symptoms. Being fully aware of yourself and your symptoms can make a tough conversation with family, friends, or medical professionals much easier. Use the self assessment tool below, provided by Mental Health America, to begin your journey towards a healthier mind.
MSIDS 38-Point Symptom Checklist by Dr. Richard Horowitz
Self-diagnosis should not be your final step towards achieving better mental health, but it can be one of the best steps you take towards recovery and a higher quality of life.
What Can You Do to Manage These Symptoms?
Seek Professional Help
While many patients may already be working with a Lyme specialist to treat their illness, if you are experiencing psychiatric symptoms, Project Lyme encourages you to consult additional practitioners. Therapists, outpatient, and inpatient programs are more accessible than ever before. Mental health professionals can assist in a variety of ways. Being judgment-free and unbiased, they can be a good person to confide in about a crisis or shame you may feel from a rage incident. Depending on your situation, they may also have the ability to put together treatment regimens specifically aimed at combating advanced psychiatric symptoms. With tele-health becoming more popular, you may even even be able to see a psychiatrist or therapist through a secure video chat platform. With growing investment in publicly offered programs, it may be more affordable than you realize.
In addition to professional help, there are a variety of additional resources available to patients to help them get through difficult times. Keep in mind you can always:
Reach Out to a Loved One
Opening up about mental health requires you to be vulnerable, especially when speaking with a loved one. The benefit is that talking to a person you trust can lead to immediate and consistent help at no cost. Depending on the severity of your symptoms, this person could help you get the care you need or just become a shoulder to lean on when things get tough.
A loved one could also help you make a list of contacts, such as other trusted friends or family members. Make sure to let these people know in advance that they are on this list so they can be prepared to rise to the occasion if necessary. In more severe situations, a list of crisis phone numbers and local resources may be a good idea.
Call a Hotline, Visit a Website, or Join a Group
Project Lyme knows that creating a plan that best fits your needs can take some time. For this reason we have compiled a short list of free, helpful resources available to you.
- National Suicide Prevention Lifeline 1-800-273-8255
- National Alliance on Mental Illness (https://www.nami.org/help) Help Line can be reached Monday through Friday, 10 am–8 pm, ET. 1-800-950-NAMI (6264) or (info@nami.org)
- Generation Lyme (https://www.genlyme.org/) is an initiative of Project Lyme that hosts weekly meet-ups supporting patients with Lyme disease.
- Depression and Bipolar Support Alliance (dbsalliance.org) hosts in-person or online support groups for people experiencing symptoms of Depression and Bipolar disorder.
Watch These Educational Webinars
Psychiatrist Jane Marke, Child and Adolescent Psychiatrist Rosalie Greenberg, as well as social worker and therapist Audrey Amir, provide medical insight along with strategies to cope. Our panelists also address frequently asked questions and seek to dispel confusion over psychiatric issues facing the community.
Neurological Lyme disease, also known as Lyme neuroborreliosis, occurs when Borrelia Burgdoferi bacteria invade the central nervous system. Some describe neurological Lyme disease as a Lyme infection of the brain. Research has found that up to 15-40% of late-stage Lyme patients develop neurological disorders. Experts Dr. Brian Fallon and Dr. Robert Bransfield discuss.

